I love working with kids. They’re these beautiful little beings that inherently trust me and most often respect my authority and knowledge. It’s a gift I tell you. A truly, incredible gift. And with that gift, comes with great responsibility, particularly when it comes to managing chronic pain. Unfortunately, I will admit that when I started working with kids, I thought chronic pain was a thing of my past. Needless to say, I was mistaken.
Kids, like adults, suffer from chronic pain too! I remember thinking to myself, “how is this even possible?” How is it possible that a 9 year old girl has been immobilized in a boot or a cast, non weight bearing, for 9 months, for a completely benign and mysterious injury?!? How is it possible that this 13 year old boy has seen 10 different doctors for lower back pain, with normal imaging and labs, only to come to see me with a year of chronic back pain under his belt? How is it even possible that these patients took so long to finally get to me? What is happening??
Hopefully we’re all smart enough to realize that the answer to these questions is immensely complicated. Currently, the literature does not support one clear answer for treating these kids and is often quite limited in its availability and robustness. However, there is one clear commonality between all of them; pain is an output from the brain and a child’s brain is more bioplastic than any other brain. What that means is that their ability to change and learn new behaviors, new coping strategies, new movements, new anything, is exceptionally good. So again, what is happening and why does it often take them so long to #GetPT1st?
I have always seen treating youth and adolescents as an opportunity. It’s an opportunity to take an individual, with a ripe ability to learn, and teach them all the incredible things their bodies are capable of doing. To teach them about pain, about their bodies, about their minds, and about their ability to overcome it. To EMPOWER them. In my personal and professional opinion, kids in chronic pain, are an opportunity to change the future of chronic pain as a whole. If they learn early to #GetPT1st and to build habits that promote a healthy life, we will have set them up for a future of success.
But it’s not always that simple. Children are influenced entirely by those around them. Their concept of pain and their ability to understand pain is limited. If the doctor says, we need an MRI, the family might think, “oh no! they have a herniated disc and they will live their life in pain all the time, just like me.” Think about that for a moment…. Think about the fear that family, and subsequently that CHILD, is experiencing when they are told the child needs an MRI for their back pain. It’s scary. To me, in working with kids, it is those moments that things get carried away and the fear avoidance model will help to explain this.
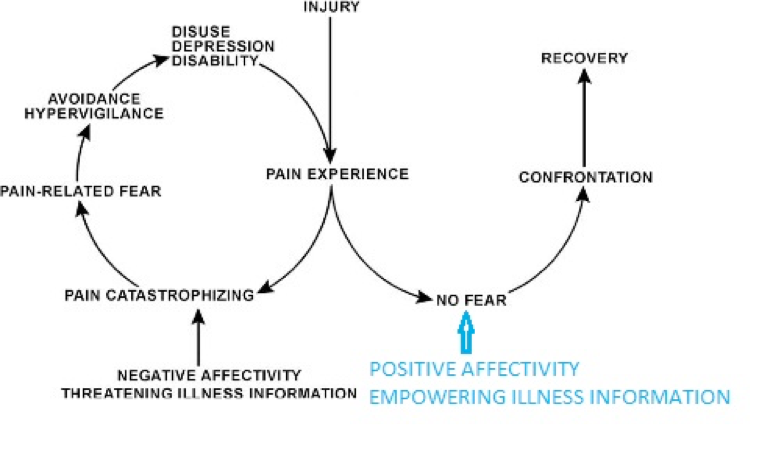
Original image: Vlaeyen J. Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 year on. 2012
The fear avoidance model is commonly used in our understanding of why things get carried away and definitely comes with some controversy. I have taken the liberty to edit this model (added info in blue) to help us understand how we all can make a difference in a child who has been experiencing chronic pain. The thing is… everyone is different and has different experiences to contribute to their recovery or lack thereof. Remembering that is essential, but the key here is that kids inherently lack those experiences. They depend on what others tell them, almost entirely. If they move towards the pain catastrophizing cycle and are being fed negative or threatening illness information, they are more likely to continue along that cycle. Physical therapists and many other healthcare providers often contribute to this avoidance cycle more than we might like to admit. I cannot tell you the number of times I hear a physical therapist tell a 16 year old to stop activity because of their pain. Or hear them say to a 10 year old what is wrong with her body. After all, this is what the medical system has trained us to do. Find the problems, tell them the problems and then fix the problems. Unfortunately, when we do this to a 10 year old, she BELIEVES us. She believes that her body is broken because you’re telling her it’s broken. The tendency for a kid to believe what you say is exponentially better than that of a 50 year old. Why? Because of experience, or lack thereof. It is vitally important that during these ripe, tender years, we are promoting patients more towards the “no fear” progression in ANY pain experience they have. By doing so, we teach them that recovery is possible, that the body is a wonderful self healer, and that their young bodies are beautiful the way they were made!
“Once you learn to quit, it becomes a habit.” -Vince Lombardi
What if after an injury or pain experience, instead of providing them with negative affectivity and threatening illness information, we inserted positive affectivity and empowering illness information. How would that change the course of their care? Personally, this little change in my practice has made significant improvements in patient progress. I believe, it is a key to a child’s success, but it all starts with who they see first. I strongly believe, if the right patients #GetPT1st, they’ll be turning the corner towards recovery faster and more cost effective.
Here’s the catch: YOU as their PT need to STOP telling them to stop. We need to tell them to go! to move forward, that motion is lotion. In line with this, as their parent, as their friend, as their companion remembering your influence on a young mind is huge and share with them…what they’re doing right? What are their strengths? What are their improvements so far? Have fun with them, laugh with them and start showing them their capabilities through movement and exercise. Learning how to trust and use the body in a way that they enjoy, that makes them feel empowered and strong. Play with them and don’t let your own self get in the way of their recovery.
Cheers,
Dr. Ellie Somers, Physical Therapist
Have questions about managing pain? Schedule an appointment today!






